Abstract
In this chapter, we present a background on the state of the art regarding Ambient/Active Assisted Living (AAL) related topics (i.e., Ambient Sensing, Medical Technology, and Geriatrics and Sociology). Later in the book we present the basis for current, new, and common technologies on the market (presented in Chapter 4), and ongoing research in AAL (examples presented in Chapter 5). The presented interdisciplinary content consists of social, engineering, medical, electrical, and mechatronics science, and together, they encompass the field of AAL, as well as eHealth.
In this chapter, we present a background on the state of the art regarding Ambient/Active Assisted Living (AAL) related topics (i.e., Ambient Sensing, Medical Technology, and Geriatrics and Sociology). Later in the book we present the basis for current, new, and common technologies on the market (presented in Chapter 4), and ongoing research in AAL (examples presented in Chapter 5). The presented interdisciplinary content consists of social, engineering, medical, electrical, and mechatronics science, and together, they encompass the field of AAL, as well as eHealth.
In recent years, AAL and eHealth have become important topics because of increased life expectancy. Even though this topic is age related, young people have already started to have a high interest in this field due to the potential for the prevention of age-related diseases.
Therefore, this chapter introduces the technological feasibility for Ambient Sensing and will be linked with the possibilities of medical technology and the necessary geriatrics background. At the end, the potential of technology of robotics in this field is presented.
2.1 Basic Knowledge in the Field of Ambient Sensing
When people enter a stage of physical and cognitive decline, typically associated with the natural aging process, the independent exercise of Activities of Daily Living (ADLs) becomes increasingly difficult [35]. If sensing and intervention technologies are not developed, this decline may progress prematurely and unnecessarily to the point when affected groups will eventually not live independently at home and become a burden on family members and institutionalized nursing-care systems. These considerations are particularly important since every emerging industrial nation is experiencing demographic change problems [36]. In this aspect, Ambient Sensing solutions could undoubtedly contribute to addressing these emerging problems.
Ambient Sensing refers to environments populated with sensors responsive and sensitive to the presence of people. An environment populated with electronic elements and microsystems can undoubtedly contribute to enhancing the independence of the elderly by introducing a degree of ambient assistance. Monitoring people’s movements in complex environments, analyzing the resulting motion patterns, and understanding people’s gestures corresponds to a high level of visual competence that can most appropriately be identified as Ambient Intelligence (AmI) [37]. Thus, Ambient Sensing – belonging to the AmI research umbrella – builds upon advances in sensors and sensor networks, pervasive computing, and artificial intelligence. Because these contributing fields have experienced tremendous growth in the last few years, Ambient Sensing has strengthened and expanded, revolutionizing daily human life by making people’s surroundings flexible and adaptive. Technologies are deployed to make computers disappear in the background, while the human moves into the foreground in complete control of the augmented environment. Ambient Sensing systems are a user-centric paradigm, supporting a variety of artificial intelligence methods and works pervasively, nonintrusively, and transparently to aid the user. They support and promote interdisciplinary research encompassing the technological, scientific, and artistic fields, thus creating a virtual support for embedded and distributed intelligence. They will eventually become invisible, embedded in our natural surroundings, present whenever we need them, enabled by simple and effortless interactions, attuned to all our senses, adaptive to users, context-sensitive, and autonomous.
The basic idea consists of a distributed layered architecture enabling omnipresent communication, and an advanced human–machine communication protocol. The Ambient Sensing paradigm sets the principles to design a pervasive and transparent infrastructure capable of observing people without interfering with their lives but at the same time adapting to the needs of the user. It must be noted that populating a home environment with sensors must be performed following a space-efficient utilization scheme. Elderly people, and especially the ones using assistive devices such as wheelchairs and rollators, require increased barrier-free space for mobility purposes.
In the following sections, an overview about the rule of vision systems as well as radio-frequency identification (RFID) technology in this context is provided in order to explain the different underlying technologies used in the realization of such systems, and their corresponding application areas.
2.1.1 Vision Systems
Vision is arguably the strongest of the senses in humans and in many other creatures. It allows us to fully understand the surrounding environment by providing spatial information of objects around us. With this amazing ability, we can determine the position, identity, and status of the various objects in the environment, so that we can interact with and react to various unexpected events. It is therefore reasonable that we attempt to give a sense of vision to the machines in order to turn them into even more useful and efficient tools. Many vision-based sensors have therefore been developed throughout the years. Three-dimensional (3D) vision systems base their operation on the collection of stereoscopic image pairs and on decoding the depth of information by examining the relative displacements of objects within a pair of images, relative to each other. This process is called stereo-photogrammetry. The observation, using our eyes, allows us to perceive the relative distance (depth) of objects that enter our field of vision. However, the human brain is the mechanism that is responsible for successfully decoding the depth information, i.e., the stereoscopic image pair, giving us the ability of depth perception. Conversely, in stereoscopic vision systems, an algorithm that can analyze the digital images taken by a stereo camera pair and recover the important depth information by sampling the areas which are illustrated in the optical scene must be devised. Depth estimation in a scene using image pairs acquired by a stereo camera setup is one of the important tasks of stereo vision systems.
Disparity map extraction of an image is a computationally demanding task; practical real-time hardware-based algorithms require high device utilization recourse usage, and depending on their disparity level operational ranges, this may lead to significant power consumption. Apart from digital camera sensors, other technologies which base their “visual” sensing performance on laser, such as Light Detection and Ranging (LiDAR), or infrared such as Depth Sensors have also been developed.
2.1.2 RFID Technology
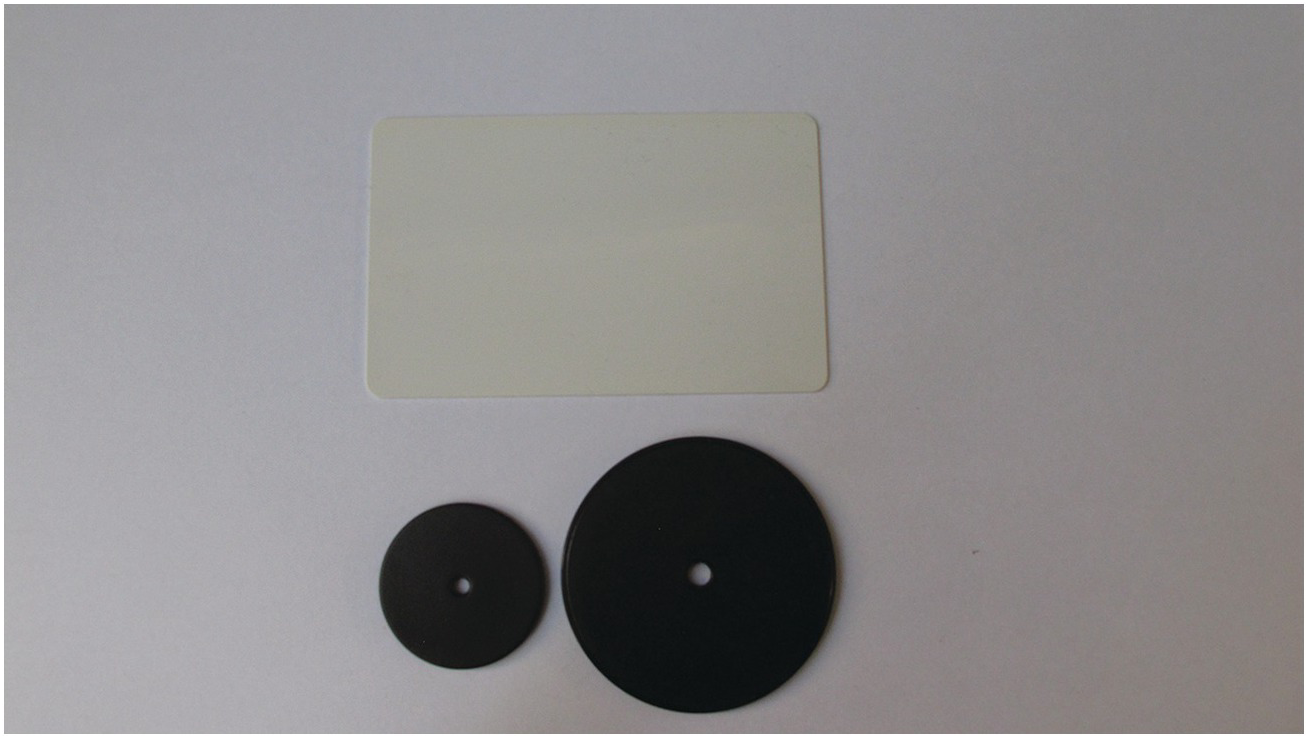
In recent years, RFID technology has moved from insignificant into conventional applications that aid in simplifying the handling of items and objects. RFID enables identification from a distance, and unlike the earlier barcodes technology, it functions without requiring a line of sight or a specific visual pattern to be detected, recorded, and processed [38]. RFID tags (see Figure 2.1) support a larger set of unique IDs than barcodes and can incorporate additional data such as manufacturer, product type, and even measure environmental factors such as temperature. Furthermore, RFID systems can discern many different tags located in the same general area without human assistance. In contrast, consider a supermarket checkout counter, where the personnel must orient each barcoded item toward a laser scanner reader in order to identify it. If all items had an RFID tag attached on them, the checkout process on the counter could have been fully automated without explicitly requiring human assistance.
Figure 2.1 Exemplary RFID Tag.
Many types of RFIDs exist, but at the highest level we can divide RFID devices into two broad classes [39]: active and passive tags. Active tags require a power source, i.e., they are either connected to a powered infrastructure or use energy stored in an integrated battery. One example of an active tag is the transponder attached to an aircraft that identifies its national origin. However, batteries make the cost, size, and lifetime of active tags impractical for most small-scale applications. Passive RFID tags are thus preferred because they don’t require an external supply source. The tags also have huge operational lifetimes and are tiny enough to fit into a practical, adhesive label.
A passive tag consists of three parts: an antenna, a processing unit attached to the antenna, and some form of encapsulation. A tag reader is responsible for powering and communicating with a tag, which is attached either to a personal computer or to a digital communication network. The tag antenna captures energy and transfers the tag’s ID. The tag’s processing unit is responsible for coordinating the communication and transmission process. The encapsulation maintains the tag integrity and protects the antenna and processing unit from environmental conditions or damage.
In a home environment, this technology can be utilized to assist elderly people by providing them with a real-time inventory of their high priority items. Experiments conducted during the proposed study, revealed the efficiency of this “invisible” technology, and the variety of potential applications to which this technology can contribute. By combining computerized databases and inventory controls linked through digital communication networks spread across the home environment and across a global set of locations, RFID technology can efficiently pinpoint individual items as they move between locations, warehouses, vehicles, and stores.
2.2 Basic Knowledge in the Field of Medical Technology
Life quality and health are very closely related to each other. It does not matter how rich or poor someone is, as soon as their health is gone, they suffer. Therapy is necessary to successfully cure a person. The type of therapy is dependent on the disease, and therefore it is a major task for a physician to identify the cause of a disease and then decide together with the patient how to recover or at least treat the disease.
Depending on the kind and stage of a disease, it may happen that the affected becomes unconscious or comatose suddenly and without any warning symptoms. This happens with diseases that have silent symptoms and break out suddenly. For example, heart attacks can be a result of a permanently high blood pressure. To treat a person, the cause of the disease must first be identified. An anamnesis (if possible) in combination with first measurements (e.g., blood pressure, pulse, glucose, and ECG) allow the physician to find the proper treatment, and sometimes to identify additional health risks. For example, type II diabetes is a typical disease, which normally in a physical examination gets accidentally diagnosed [40] by a physician because of other reasons. However, this means regular physical examinations increase the chances to recognize the beginning of a disease at an early stage, where the chances of a cure are high. The field of medical technology therefore focuses a lot on identifying diseases.
More people, old and young, are aware of these facts. Therefore, wearables, which measure physiological parameters, have successfully entered the consumer market. Wearables, however, tend to be forgotten to wear, and many people feel that wearing them all day is inconvenient. In order to improve health screening and to increase the security of the user, a new strategy has started in this field of research: the unobtrusive implementation of health sensors in the environment.
Sensors must be noninvasive for both physicians and patients and designed to work in the background when implementing health sensors into the user environment. In the following sections, devices used for noninvasive diagnostics are introduced, which are highly interesting because they can be unobtrusively implemented into the user’s environment. The possibilities are too large to present every type of measurement; however, we will give an overview of the most important measurements with regards to AAL and eHealth.
2.2.1 Pulse Oximetry
Pulse oximetry is used to measure pulse and oxygen saturation at the same time. To do this, a sensor has to be attached on the earlobe or finger [41], or at the heel for newborn and premature babies. The sensor consists of a light sensor and an emitting source. There are two possibilities of how the sensor measures and receives pulse and oxygen blood saturation data: either by the transmission of the tissue from the emitted light, or by remission (see Figure 2.2).
Figure 2.2 Left: Exemplary sketch of pulse oximetry on the earlobe with light transmission.
Right: Exemplary sketch of pulse oximetry on the finger with light remission.
The pulse is then counted by the arrival of the absorbed light on the photodiode. The emitted light gets absorbed by a blood wave, which is passing by the measurement spot. Usually for this technology, an LED-emitting light to a photodiode is used [42]. To make the signal usable, a power amplifier is normally used for an analog low-pass filter, which amplifies the signal [43].
To measure the oxygen saturation of the blood, two LEDs are necessary: one should emit light at 660 nm (red light), and the other LED at 950 nm (infrared). The reason for this is due to the extinction coefficient of blood (shown in Figure 2.3, data source [44]). When saturated with oxygen, the erythrocytes absorb more infrared light and absorb less light at 660 nm. The 950 nm LED is used to get a relative value for the reference measurement Hb, whereas 660 nm is used for the HbO2. Using Eq. (2.1) allows for calculating the precentral saturation in relation to the overall hemoglobin.
 (2.1)
(2.1)However, this sensor has two weak points; heavy movements can easily disturb the measurement and, at the end, the device can only detect how much of the blood is saturated. Normally the oxygen is binding with the hemoglobin, which the erythrocytes carry. However, other gases like carbon dioxide bind much more strongly than oxygen to the blood. This leads to a perfect measurement result, although the blood does not carry oxygen. This dangerous life situation, which, for example, can occur in response to a fire gas intoxication, cannot be detected using this technology.
Figure 2.3 The extinction coefficient of unsaturated hemoglobin (Hb), and hemoglobin saturated with oxygen (HbO2).
Also, smoking can lead to wrong results. A person who smokes during a measurement period will have 100 percent saturation. However, the true saturation will be visible after some time and will drop to around 95 percent. In [41], the following thresholds for pulse oximetry are defined: A healthy person normally has 95–100 percent saturation. People who have 94 percent saturation or lower normally suffer from hypoxia and need treatment. People with a saturation of less than 90 percent are a medical emergency case.
2.2.2 Blood Pressure Meter
Those who have used a blood pressure meter know that the device gives three values: the systolic blood pressure, the diastolic blood pressure, and the pulse. In the past, physicians and caretakers measured the blood pressure by palpation (according to the Riva–Rocci method) with a cuff. Therefore, e.g., the caretaker, or physician, must find the pulse, e.g., on the wrist of the patient. Once the pulse has been found, the cuff, placed on the upper arm, gets pumped (using a small hand pump) until the pressure is large enough to close the brachial artery [45]. This stops the blood flow to the hand, which is not very convenient if the pressure is high for too long.
Of course, now there is no noticeable pulse. Slowly opening the valve on the cuff leads to a slow reduction of the pressure, which the cuff uses to close the artery. The nurse, or physician, has to wait until the first pulse wave is noticeable on the wrist: this is the blood pressure that is strong enough to open the artery for a very short moment. This value is called the systolic blood pressure. This value is the highest pressure and marks the pressure occurring during a heart contraction.
However, there is also a constant low blood pressure while the heart is not contracting. This value is known as the diastolic blood pressure. To also measure the diastolic value, physicians and caretakers use a stethoscope to hear the Korotkoff-sound (auscultatory measurement).
These Korotkoff-sounds, which sound similar to a heartbeat but are of distinct origins, are the result of turbulences, which occur when the cuff is narrowing the artery (see Figure 2.4) [46]. As soon as the vessel is able to send blood through the occlusion (caused by the pumped cuff), this sound occurs and marks the systolic value (as it is with the palpatory measurement). The Korotkoff-sound stops as soon as the turbulence stops and the blood continues with a laminar flow, which is achieved as soon as the pressure of the cuff is weaker than the lower blood pressure (the diastolic value). This means that the last Korotkoff-sound the physician or caretaker hears, while reducing the cuff pressure by the valve, marks the diastolic blood pressure.
Figure 2.4 Left: No blood flow, because the cuff pressure is higher than the systolic blood pressure. Center: Turbulence blood flow, which causes the Korotkoff-sounds, because the cuff pressure is between systolic and diastolic blood pressure. Right: Laminar blood flow, because the cuff pressure is lower than the diastolic blood pressure.
However, both methods (palpation and auscultation) are very subjective measurement methods dependent on the sensibility and hearing abilities of the person taking the measurement. Herein, this measurement method has been automated. The device in principle consists of an automated pump and a pressure sensor (e.g., a capacitive pressure sensor) measures the pulse. The device pumps the cuff to close the artery and then stepwise reduces the pressure (as depicted in Figure 2.5). Once the cuff has a larger pressure than the cuff, the pulse oscillation increases, which the blood pressure meter marks as a systolic value. Once the oscillation strength returns to its normal level, the device marks the cuff pressure as a diastolic value.
Figure 2.5 Exemplary sketch describing the working principle of a blood pressure meter.
However, the most precise method to measure a blood pressure is the invasive blood pressure measurement. Here, the pressure sensor is not attached to a cuff; it is directly attached via a catheter or cannula to the arterial blood. Using this method allows care staff or a physician to differentiate the blood pressure in the region and system. The blood pressure meters, as described in this section, measures the high-pressure system. However, the blood pressure of the veins belonging to the low blood pressure system is not measured by the commercial devices [47].
Normally the blood pressure should give a result of 100 mmHg up to 140 mmHg (optimal 120 mmHg) for the systolic, and less than 100 mmHg for the diastolic blood pressure value. However, the blood pressure is also dependent on the body region, as well as of the kind of blood pressure system.
2.2.3 Temperature Measurement
The body temperature is a physiological parameter, which can change according to the environment or the health condition. An increased temperature, caused by diseases like influenza, is called a fever. Often, a fever is part of the defensive response of the immune system, with the objective to kill intruding microbiological organisms like bacteria or viruses [48]. Although this means that a fever is supporting the curing process, a fever can be dangerous if the temperature is above 43°C [49]. Therefore, a fever is a good measure of someone’s health. For the elderly, it is specifically important since high fever can harm the cardiovascular circulation, and this often needs to be suppressed.
To identify a fever, touching the forehead may be enough. However, this can be a very imprecise method. Fortunately, fever measurement devices are very cheap, and nearly every drugstore sells such devices. Mercury-in-glass thermometers (see Figure 2.6), which measure the temperature related expansion of the liquid, have now been replaced by the most common digital version (see Figure 2.6) of this measurement device (which measures by a thermistor). The disadvantage of these devices is the fact that they need up to 5 minutes to receive a result. Measurement areas are axillar, oral, and rectal, whereas axillar is not considered to be the most precise measurements area [50], but the axillar measurement is one of the most convenient measurement areas. Of course, there are also other measurement areas, which are quite inconvenient or even painful, e.g., rectal [51].
However, user impatience (especially in small children) often leads to false measurement results. Therefore, devices which measure the fever very fast and reliably by infrared on the eardrum ([52], [53], [54]) now exist. However, there is a high risk with this device related to wrong measurements, e.g., by wrongly holding the tympanic fever measurement device, which is then measuring the meatus, instead of the ear drum. An additional disadvantage is that all the mentioned body temperature measurement methods or devices need direct body contact, which leads to hygiene problems. For example, [55] points out the importance of sterilizing these devices, if they are to be used for more than one person.
Therefore, thermometers which measure fever on the forehead without direct contact by infrared also exist. Depending on the environmental temperature, the accuracy of this kind of measurement may be compromised [56], [57]. On the other side, these kinds of devices allow a fast and hygienic measurement of the body temperature. In the last years, this aspect of fast and hygienic measurements became very important not just for the health care, eHealth, and AAL sectors, but also with regards to travel of tourists and business people through different climatic areas. Traveling brings together people of different immune system strengths, which in return supports the development of epidemics and pandemics (e.g., the influenza pandemic in 2009 [58]). Since influenza is a health and even life risk for the elderly [59], thermal cameras have been used at airports for quick mass screening [60]. Therefore, it is not surprising that there are several studies (e.g., [61], [62], [63]), which have investigated the usage and reliability of thermal cameras for fever measurement.
2.2.4 Glucometers and Their Measurement Possibilities
Type II diabetes is the most common metabolic disease in the world, which can lead to blindness and limb loss [64]. Therefore, Glucometers have become important devices in a lot of homes. The general measurement principle is normally based on enzymes, which react only with the sugar molecules in the blood.
According to [65], the enzymes are immobilized on a platinum electrode, which must get in contact with the blood. The enzymes will then react (oxidize) with the glucose and release electrons. The glucometer finally measures the current when the freed electrons pass the device to equalize the potential difference of the electrodes. The current is proportional to the glucose concentration in the blood.
The enzymes and the electrodes are one-way products, and mostly sold as strips, which get connected by plug and play into the glucose meter (see Figure 2.7). The analysis is normally done by the glucometer itself. To get out the blood drop, the user must pierce the skin to get blood out of the capillaries (i.e., minimal invasive measurement). As the end user normally prefers to centralize functions in one device (instead of having several measurements at home), add-ons which use the smartphone to display the result exist.
However, although this method is reliable in measuring the blood sugar level (very important especially for people who are consuming insulin), this method is very inconvenient. Alternative measurement methods have been investigated. A new product to receive the same results is the glucose scanner, which must be held next to a patch. The patch itself consists of a very small needle and a small circuit, which measures and transmits the results as soon as the scanner is close enough. The patches must be replaced only once every two weeks, thus reducing injury to the skin.
However, as diabetes starts mostly silent (i.e., without clinical symptoms [40]), there is an interest to measure just for prevention. With diabetes, there is no big alternative to pricking the skin daily, but for people who just want to prevent diabetes, this is unacceptable. An alternative to checking blood sugar is checking sugar levels in urine. If the sugar concentration in the blood exceeds the renal threshold of ~180 mg/dl, glucose will be excreted in the urine. Normally a urine test stripe can prove glucose exists in the urine by an enzyme reaction, which changes the color accordingly.
In Japan, toilets are equipped with the glucometers to measure the glucose in the toilets (see Section 4.3).
2.2.5 Electrical Biosignals
Up-to-date electoral biosignals are one of the most important, non-invasive measurements methods. The electrocardiogram (ECG) is probably the most used; many are used in hospitals as well as in emergency departments. The ECG measures the sum of the electrical potential of all heart cells. The measurement of the Einthoven triangle was defined by Einthoven in 1913 [66]. The signal is measured on the hands and on the left feet, as shown in Figure 2.8.
Figure 2.8 Possible electrode placement areas for Einthoven and Goldberger lead measurements.
Since the generated signal is very weak, a differential amplifier linking two electrodes with each other is used. The measurement vector then determines the amplitude, and the more parallel it is to the electrical heart vector, the higher the amplitude is (see Figure 2.9).
Three measurements to investigate the current activity are possible with these three leads. Following the definition of Goldberger, the augmented voltage leads aVR, aVL, and aVF (see Figure 2.10), which allow a more detailed investigation, have been introduced. Of course, there are more possibilities to investigate the heart using only ECG by appropriated electrode placing (e.g., according to Wilson, Caprera circle [67], and Nehb [68]). The ECG has already entered the private eHealth market via several devices like jogging watches, where the pulse button and the watch back are electrodes, or in training devices like ergometers (e.g., embedded in the handlebars).
The difference between the ECG and the electromyogram (EMG) is in the embedded filters. The EMG is normally much stronger in the signal of the ECG and normally filtered. EMG works the same as the ECG but focuses on detecting the electrical signal of the muscles. The EMG is an important sensing device in the medical area and also in the future of eHealth and AAL. For example, the first implementation can be found in exoskeletons, which serves, for example, as orthosis [69] [70].
The Electrooculography (EOG) and the Electroencephalography (EEG) are mainly used for investigating sleeping behavior (e.g., the EOG is used to identify the rapid eye movement (REM) phase, and the EEG for the deep sleeping phase [71]), or for neurological diagnosis (to identify epilepsy, etc.). As can be seen in Figure 2.11, the EEG electrode placement is more complex compared to the six-channel ECG (shown in Figure 2.8). The electrodes (A1 and A2) on the earlobe represent the reference electrodes. The other electrodes measure toward A1 and A2, whereas the electrodes placed on the left hemisphere of the head correspond to A1, and the electrodes placed on the right side of the hemisphere correspond to A2.
However, also in the field of the EEG, a lot research focuses on the brain computer interface (BIC), which aims to control computer by thoughts. The BIC devices are already on the market; however they are not designed to control the computer but instead to allow further research on it. They consist of active electrodes (and much fewer electrodes, because here a 19-channel investigation is less important), which allow for dry measurement and measurement through the hair. The active electrodes also exist for the ECG, which allow an easier implementation into the home environment. However, active electrodes are very sensitive and unfortunately catch more noise easily. Therefore, it may also easily happen that eye movements disturb EEG measurement.
2.3 Basic Knowledge in the Fields of Geriatrics, Sociology, Etc.
As mentioned in Chapter 1, not only is the old age itself the cause of the problems, but also the multimorbidity and the resulting diseases, which reduce the quality of life and potentially lead to death. In Chapter 1, it was also mentioned that aging is not programmed, but it is an evolutionary result. In this chapter, a more detailed explanation of what exactly happens when we age, as well as what typical diseases are awaiting the aging person (and causes multimorbidity) is provided. Also, aspects of possible prevention will be discussed for the briefly summarized diseases.
The prevention aspects of the diseases mentioned in this chapter are of major importance for AAL because it is by them that life quality and the work force for the society remain preserved. Considering the social development (see Section 1.2) which showed that the number of elderly will increase while at the same time the population of young people will decrease by 2050, it is envisaged that there will be much higher retirement ages. Therefore, to keep the quality of life and the work force that the future generation of seniors can sustain for the predictably extended work life, early prevention is a key part of AAL, and must consequently involve the young generation.
Although aging is not programmed in the genes, the genes definitely have an impact on the aging progress. A very rare disease, which proves this theory, is called progeria [2]. Progeria is a disease caused by gene defects and affects DNA repair mechanisms, replication abilities, or the chromatin structure. Progeria can be differentiated into different kinds, Wiedemann–Rautenstrauch syndrome, Hutchinson–Guilford progeria syndrome, Werner syndrome, etc. However, all these kinds of progeria are segmental, which means that the different aspects of the (accelerated) aging process are differentially accelerated. The life expectancy is reduced to ~20 years, because of the age-related fragility, disease, and multimorbidity, which already start in childhood.
According to [2], genes influence roughly one-fifth up to one-third of the aging process. The other influencers consist of environmental factors (toxins, radiation, health nutrition, etc.) and happenstance. The telomere at the end of the chromosomes, for example, are known as the “biological clock.” With each cell separation, the telomeres become shorter, until they are nearly vanished. In that case, the cell loses the ability to replicate (i.e., to replace another cell). These cells are called senescent cells. Depending on the cellular stress (which means, how often a cell in a specific tissue must be replaced because of environmental factors), the time it takes a telomere to shorten changes. The more often and faster the cells must replicate, the faster the telomeres become shorter. Other additional known reasons of the aging process at the cellular and molecular level, according to [2], include:
Antioxidant protection mechanism;
Amount of senescent cells;
Accumulation of wrong processed or damaged proteins;
Accumulation of mutations, especially with mDNA;
Modification of the hormonal metabolic regulations, especially of the hormone Insulin/IGF.
Because of environmental factors like toxins and nutrition intake, etc., and the metabolic speed, the body, or organs, must replace cells in different amounts and frequency. This leads to different accelerations of the aging process from individual to individual, or even from organ to organ of the same individual.
Von Zglinicki [2] described the physiological changes while aging as follows: at the beginning, there are related function restrictions only noticeable under stress. The functional changes of the heart lead to a reduced exercise capacity. The reduced protection mechanism leads to an increased susceptibility to infections in the lungs, or to a higher aspiration risk (because of a too weak cough reflex). Additionally, by the loss of functionality of B- and T-lymphocytes (immune cells of the specific immune system, which offers the main protection for an individual in a specific climate area), the susceptibility to infections, cancer, and autoimmune processes are increased. The functionality of the kidneys and the metabolic activity of the liver are also reduced. Hormonal and neuronal steering and regulation processes are also changing and lead to different sleeping rhythms, reduced reaction time, and memory disorders. The changes in bone structure increase the probability of fractures. The reduction of the capability of the sensory organs and at the same time reduction of muscle strength increase the risk of accidents. Finally, the skin is also affected. The subcutaneous tissue including the capillary vessels and sweat glands are reduced leading to a reduction of sweat and fat production, as well as to a slowed down healing process. The turgor (inner cell pressure) and pigmentation (caused by degenerated skin cells) are also reduced leading to the typical look of the aged skin.
As it can be seen, the aging process leads to a continuously increased fragility, which sooner or later leads to unavoidable age-related diseases. The chosen diseases are introduced and briefly discussed since they are triggered by the factors mentioned in this section and lead to the reduced quality of life.
2.3.1 Metabolic Syndrome
The cardiovascular diseases are a summary of several heavy diseases. Mostly, these diseases start with the metabolic syndrome (also called the deadly quartet). According to [72], the deadly quartet consists of obesity, glucose intolerance (e.g., by Type II diabetes, see Section 2.3.3), hypertriglyceridemia (metabolic disorder of high blood level of triglycerides, which is a specific body fat), and hypertension (high blood pressure). The main trigger of this deadly quartet is obesity, which leads to hypertension and hyperinsulinemia (often occurring in Type II diabetes).
Therefore, [72] proposed that prevention of obesity has a larger impact than exercising, antihypertensive drugs and dieting. The metabolic syndrome occurs mostly in industrialized nations, which allowed the conclusion that this disease is triggered mainly by less activity and wrong nutrition intake. Sweet drinks like soda seem to support the obesity process very strongly, according to [73]. Additional to the physical activity and the food/drinking behavior, a too little/inefficient sleep schedule supports the development of obesity too [74]. Of course, it would be too easy to think that all obese people can improve their life quality by improving their daily habits. However, other factors influence obesity as well, genetic aspects, several diseases, side effect of some drugs, etc. Nevertheless, physical and mental activity with healthy food/drink and adequate sleep behavior strongly support the prevention of obesity.
The main issue on the metabolic syndrome and the following diseases is that they are largely symptom free. As soon as the first symptoms occur, it is mostly too late to rescue the life quality of the affected. Therefore, wearables are fast entering the public market, because they support people who are already actively preventing these age-related diseases. However, a weak point of wearables is that they work properly only if worn nearly always, which can quickly become inconvenient for the user. Therefore, a new approach in the research of AAL is the unobtrusive implementation of sensors for unobtrusive health analysis, which enables a seamless health check record, even if the wearables are sometimes not used (as already mentioned in Section 1.1).
2.3.2 Consequences of the Deadly Quartet
If someone is ignoring the result of the AAL devices, or is generally not screening his health status, the metabolic syndrome will lead to more serious diseases. Mainly, high blood pressure will damage the vessel walls of the arteries, leading to the development of occlusions (also known as stenosis). Depending on the region of the affected vessel, different diseases start, e.g., the peripheral artery disease. Commonly, legs are more affected than arms. The undersupply by a thrombus leads to pain while walking (also called claudication), and later to permanent pain in the affected extremity. If no improvement by medical treatment occurs soon, ulcers/gangrenes occur, meaning open wounds which are not healing/closing anymore. Sometimes it can happen that the thrombus is losing from the vessel wall and this leads to an embolus. If the embolus enters smaller arteries, an acute limb ischemia can be triggered (sudden stop of blood flow) [75]. If this condition stays untreated, the affected will lose the extremity by tissue necrosis.
Of course, the veins can also suffer under the metabolic syndrome. However, if here an occlusion is growing, the situation is even more dangerous than in the peripheral artery disease. This disease is also known as phlebothrombosis. While the affected extremity is normally white and cold in an acute limb ischemia, here the affected extremity seems blue and hot, and the skin is under great tension. Of course, here also, the affected can lose the whole extremity. However, it can also happen again that the thrombus will break lose from the vessel walls and become an embolus. Although the phlebothrombosis vanishes, this is a very dangerous life situation, because the embolus will pass the right heart atrium and ventricle, and enter the small blood circulation. As soon as the embolus enters the pulmonary artery, a lung embolus starts, which can end lethally. In [76], it is mentioned that between phlebothrombosis and the possible resulting pulmonary embolism much evidence exists that obesity increases the risk of disease.
If the occlusion is occurring in the coronary artery, this disease is called coronary artery disease, or myocardial infarction (also known as heart attack). Beside the metabolic syndrome, the risk of disease on a heart attack can additionally increase by stress, left ventricular hypertrophy, total cholesterol, and smoking [77]. Finally, also the vessels for the brain supply can be affected, which leads to a stroke (also known as cerebrovascular accident/insult). Here also, smoking additionally increases the risk of diseases on a stroke. The metabolic syndrome mainly increases the risk for an ischemic stroke. However, intracerebral hemorrhage is also possible, e.g., as a result of a ruptured aneurysm. However, for strokes, the ischemic strokes are dominant [78]. In both cases (heart attack and stroke) there is a similar pathomechanism; the blood supply to the heart or brain tissue behind the occlusion (caused by a thrombosis or embolus) is interrupted leading to a necrosis of the affected heart or brain cells. This first reduces the function of the affected organ, and finally leads to the death of the affected person. According to the [79], the main statistical reasons for death are listed in Table 2.1.
Table 2.1 Death Reasons according to ICD-10 in 2014 [79]
As it can be seen in Table 2.1, chronic ischemic heart disease, which can be seen as secondary diseases of the deadly quartet, is the number one reason of death. However, not only is the number one related to the metabolic syndrome, but also numbers two, four, seven, and ten. Counting the amount of dead people together gives an impression of the real victims of the deadly quartet.
2.3.3 Diabetes Mellitus
Type II diabetes (also called adult-onset diabetes), is totally different from Type I diabetes, and theoretically curable. Type I diabetes is an autoimmune disease, where the immune system attacks the islets of Langerhans of the pancreas. The islets of Langerhans (also known as pancreatic islets) are responsible for the endocrine function (i.e., the production of insulin and its injection into the blood). Once the immune system has destroyed all islets of Langerhans, insulin production stops, and if untreated, will lead to death. Fortunately, by frequently using injections of the insulin hormone, the diseases can be treated (although not cured) and the life expectancy of the diseased is nearly unchanged. People suffering from Type I diabetes are mostly very slim, as insulin is not only responsible for the absorption of sugar into the cells, but also stops the transfer of fat into sugar. As Type I patients do not produce insulin, fat gets immediately transferred to sugar by biological processes in the cells. Being an autoimmune disease, genetics are mainly responsible for the disease. However, the immune system is normally triggered mostly by unknown environmental factors.
Type II diabetes is completely different. The islets of Langerhans operate normally. This means that the affected patients produce insulin. However, the cells of the affected are oversaturated with sugar and start to ignore the hormone (i.e., Type II diabetes is an insulin resistance disorder) [80]. This leads to a vicious cycle, because at the beginning, the body compensates this problem by producing more insulin until the cells react. However, this will increase the insulin inhibition of the cells. Sooner or later, there is permanent insulin in the blood, which also permanently stops the transfer of fat into sugar. This then means that each gram of fat will be stored, and this is what finally leads to obesity. The high sugar concentration in the blood additionally changes the osmotic pressure, the liquid of the cells gets into the vessels and leads finally to an increased blood pressure. This pathomechanism leads again to the metabolic syndrome as already explained in Section 2.3.1. The use of insulin injections, as it is used in Type I diabetes, is only a patchwork to reduce the sugar concentration in the blood, but it also supports the obesity process.
Nevertheless, Type II diabetes is curable by lifestyle change. The same prevention as described at the beginning of Section 2.3 is necessary. Diet (especially the reduction of sugar consumption), until the metabolism of the body is recovered, and less sugar intake compared to the normal behavior, combined with appropriate physical activity, could cure the disease. G. Herold [81] expressed that body weight normalization can avoid or at least slow down the progress of Type II diabetes.
Unfortunately, in industrialized nations, the diseased person, sooner or later, will use insulin or other medication.
2.3.4 Osteoporosis
Osteoporosis, a disease of the bone structure, consists of two main features: reduced bone density and bone quality (i.e., increased fragility) [82]. The bone marrow fills the human bones, but in the regions where no bone marrow fills the bones, normally a spongy bone structure is found. This structure allows a highly robust, yet very light bone architecture. If the bones would consist only of compact bone substance, the body weight would significantly rise. This lightweight construction of the bone structure allows that just 15 percent of the human body weight is caused by the bone structure.
The bones are permanently rebuilt. While osteoblasts construct the bone, osteoclasts destruct the bone structure. This allows the bones to adapt to the environment, e.g., increasing bone substance if necessary, or decreasing if the person is too inactive. For example, if an astronaut is in the space, the muscle and bone structure decreases, because of the missing forces on the tissue (caused by the weightlessness) [83]; gravity is a necessary stimulation to increase the bone density. Also, in old age the bone structure is slightly reduced, which is also one reason why it is easier for the elderly to break a bone. However, if the bone structure decreased significantly, the affected become highly fragile (osteoporosis called). A typical break point is the femoral neck.
In most people, the exact reasons triggering primary osteoporosis are unknown. It is assumed that postmenopausal estrogenic absence is an important factor in osteoporosis development [84], which is one reason why females are more often affected than males. Secondary osteoporosis is mainly caused by influenceable factors, hyperthyroidism, steroid therapy, Type II diabetes, very sweet drinks with acid (sodas), heavy caffeine or chocolate consumption, smoking, fashion trends like thigh gaps and slimness, etc. [82], [85].
However, other factors can also trigger this disease, disturbed cortisone, or calcium metabolism, lack of sex hormones (in males), Type I diabetes, lactose intolerance, chronic indigestions, etc. In young age, the disease can nearly be cured by changing the lifestyle through training, avoiding nicotine, reducing fall risk (prevention of fractures, which would lead to immobilization) and medicine (calcium, vitamin D [82], osteoclast-disturbing drugs, etc.). However, the disease progression can only be slowed down, or stopped, but the existing damage on the bone structure cannot be fully reversed.
Osteoporosis leads also to a typical shape, which is caused by broken vertebral bodies. The typical “s” shape of the spinal column is amplified, while at the same time the body height is reduced. The stomach gets shifted to the front and a humpback grows (see Figure 2.12).
2.3.5 Parkinson’s Disease
Parkinson’s disease normally starts around 50 years of age (or older). However, there is a minority who become affected much earlier (from 30 years of age) [86]. Furthermore, in cases where the disease is inherited, it starts earlier (~40 years of age). This disease is becoming more prevalent due to demographic changes (see Section 1.2). Pesticides and posttraumatic occurrences, infections, and misused drugs are other known causative possibilities. However, the reason for developing Parkinson’s disease is mostly unknown. The pathomechanism is as follows; loss of nerve cells of the substantia nigra, which is an area located in the brainstem and responsible for the production of dopamine hormone, in the diseased leads to a lack of dopamine. The first symptoms occur as soon as significant dopamine levels are missing in the blood.
The cardinal symptoms are: tremor (usually rest tremor), rigidity (also known as lead-pipe or cogwheel symptom), akinesia (or bradykinesia), as well as the loss of postural reflexes [87]. However, other symptoms, e.g., blister disorder, visual disorder, sensory disorder, sexual dysfunctions, sleep disorder, and psychological changes can occur while the disease progresses. Typical symptoms include gait disturbance, sparely gesture and mimic, small handwriting and dysarthria (disorder of the speech motor activity).
Parkinson’s disease belongs to the degenerative nerve diseases, which cannot be cured. Dopamine injections have no curing effect, as the blood-cerebral barrier filters this hormone. Fortunately, the pre-stage of dopamine, called L-Dopa [88] (levodopa), can pass the blood-cerebral barrier and thereby enter the brain. This drug at least slows down the disease progression. The use of deep brain stimulation can additionally reduce the symptoms, however, it is dangerous, as needle electrodes must be inserted through the healthy brain areal up to the substantia nigra. Nevertheless, these interventions do not stop the progression of the disease but can only slow down the disease and eventually the affected becomes hospitalized.
2.3.6 Dementia
Dementia is a collective word for several diseases of the brain. One of the most well-known diseases increasingly becoming more prevalent because of an aging population is Alzheimer’s disease. Here, the brain (especially the hippocampal region) is affected mostly by underdevelopment [89]. This degeneration is caused by the collapse of several axons of the nerve cells. The embedded tau protein then produces plaques. The plaques, additionally, disturb the signal transmission on the remaining functional synapses.
The reduced volume of the gray tissues, which mainly are the processing nerve cells, while the white nerve tissues are mainly responsible for information transmission. Additionally, the ventricles are enlarged, causing a reduction of the brain volume.
The main known symptom is memory reduction (especially the short-term memory), but also disorders of orientation and time perception are usual symptoms. The practical skills are limited, and the communication abilities reduced. Unfortunately, for Alzheimer’s disease, there exists no cure. The progression of Alzheimer’s or other dementia diseases can be slowed down by some drugs (e.g., acetylcholinesterase) and by cognitive training. In [90], it is even mentioned that cognitive training should be used to prevent Alzheimer’s as early as possible. The prognosis of Alzheimer’s disease is that within six years (on average) the affected will die [91].
2.3.7 Sensory Organs: Eyes and Ears
In addition, our sensory organs also suffer during aging; it doesn’t matter how good the eyes of a person are, the eyes seem to get weaker with age (Presbyopia). The reason is that the accommodation strength (i.e., the variable optical refraction power of the eye) of the lenses is reduced since the older a person becomes, the more the water in the core of the lenses reduces. This further leads to reduced elasticity and is the reason for the reduction in accommodation strength. For example, young people have an accommodation ability of 14 dpt, while a person of ~45 years has only 3 dpt left [92].
Some elderly may have bad luck, e.g., by a disturbed metabolism. If glucose crystals get stored in the lenses, the liquid will be bounded to the crystals resulting in secondary cataracts. Here, a predisease (e.g., Type II diabetes) triggers this condition. Of course, the standard cataract can occur without diabetes, and may be caused, e.g., by X-ray, ultraviolet light, electric current, and also punch or stab injuries. A cataract is characterized by the swelling and clouding of the lenses [93] (which changes the image recognition of the human eye as depicted in Figure 2.13). These events finally lead to complete blindness of the affected eye. Although it is possible that only one eye is affected by a cataract, the second eye, sooner or later, also becomes affected. A cataract is curable by replacing the diseased lens with an artificial lens.
Left: an image as seen by a normal person.
A more serious disease is glaucoma. In this disease, the drain-away of the anterior chamber is blocked leading finally to very high intraocular pressure. The result is that the nerve cells on the retina suffer from the two large intraocular pressures, which leads to disturbance in image recognition (see Figure 2.14), as well as blindness in the end stage [94]. Ignoring secondary glaucoma triggered by infections or traumata, glaucoma is distinguished as either open-angle or closed-angle glaucoma. In closed-angle glaucoma, the angle between the cornea and iris is too narrow (e.g., due to thick lenses), so that the liquid within cannot drain (via Schlemm’s canal). In open-angle glaucoma, the drain-away is blocked directly by degenerative changes in the Schlemm’s canal, or to be more precise, at the surrounding trabecular meshwork. Medication is available for the regulation of the ocular pressure, and another treatment option today is the use of LASER to create an artificial drain-away canal.
Left: an image as seen by a normal person.
Even more serious is age-related macular degeneration. Generally, there are two different types of age-related macular degenerations existing: dry and wet [95]. Usually, affected people (up to 85% of the age-related macular degeneration) suffer from the dry version of the disease. Here, metabolic end products get deposited between the retinal pigment epithelium and the blood vessels (called drusen). This then leads to an undersupply of the nerve cells of the retina behind the drusen, resulting in necrosis of the affected retina tissue. When the macula lutea (yellow spot), which is the area on the retina where most nerve cells for visual reception exist (i.e., where the lens focus the light, so that a human can see sharp), is affected, the diseased person loses visual acuity (see Figure 2.15).
Left: an image as seen by a normal person.
Right: the same image as seen by a person with age-related macular degeneration.
Additionally, up to ~15 percent of macular degeneration patients suffer from wet macular degeneration complications. Here, the progression of the disease is accelerated by vessels that grow through the retina pigment epithelium, which supply the nerve cells with blood. Unfortunately, these vessels lead to an additional uplift of the retina pigment epithelium and are also more permeable than normal vessels (this causes fluids to entering into the interstitium and additionally support the lift up of the nerve cells of the retina). By LASER therapy (or alternative photodynamic or by antibodies), the progression of the wet macular degeneration can be slowed down. However, the disease progresses faster than the dry macular degeneration. In each patient, the disease progresses differently and normally affects both eyes.
According to the famous picture by La Fée Électricité in Musée d’Art Moderne de la Ville de Paris (from Raoul Dufy for the International Exhibition 1937), when the human environment became bright and loud due to electricity, Raoul Dufy let her run away, while the Fée Électricité covers her ears (visible on the left side of Raoul Dufy painting). Furthermore, besides the eyes, the ears also get weaker in old age, proving that Dufy was right with his painted prognosis that the future will become bright and (too) loud.
People who live in very quiet areas (e.g., deserts) keep their hearing ability up to high age. The “natural” loss of hearing ability is frequency related. Newborns and children can hear in the range of frequencies from 16 Hz up to 16,000 Hz, however, the ability to hear at higher frequencies (>10,000 Hz) reduces with increasing age [96]. Age-related hearing loss (i.e., deafness and presbycusis), are a result of (or at least partially responsible for) chronic noise damage to the ears, i.e., from loud environments [97].
The ear can be split into three areas; outer, middle, and inner [97]. The middle and inner ear consist of the interface which converts a mechanical air pressure wave into an electrical signal (also called mechanoelectrical transduction) via the eardrum, which is the smallest bones in the human body, hammer, anvil, stirrup (middle ear), and the cochlea (inner ear in combination with nerves). In the cochlea (see Figure 2.16), hair cells get stimulated by the tectorial membrane after getting into oscillation through the basilar membrane. The basilar membrane triggers the tectorial membrane by the traveling wave triggered by the oval window (also visible in Figure 2.16), which is the interface to the stirrup.
Figure 2.16 The tympanum and its connection to the cochlea via the hammer, anvil, and stirrup, which connects the ear drum and the oval window and enables mechanoelectrical transduction in the human ear.
According to the tube of the cochlea and its resonance frequency characteristics, only the hair cells (which belong to the corresponding frequency) on a specific spot get stimulated. These hair cells then translate the mechanical pressure wave into an electrical signal. If the middle ear gets destroyed because of disease (the eardrum is broken, etc.), the person loses their hearing ability. However, if the hearing capability via bone conduction is unchanged good. If the hair cells are destroyed because of exposure to extensively loud sounds over a long period of time, e.g., loud music, then the hearing ability suffers from air and bone conduction.
However, the bone conduction allows to bypass the middle ear and to send sound directly to the inner ear [97]. A common area to place a hearing aid, which is working via bone conduction, is the mastoid. Of course, in case the inner ear is damaged, the hearing aid via bone conduction does not improve the hearing abilities compared to hearing via air conduction. Hearing aids consist basically of a microphone, a microchip responsible for capturing the audio signal and forwarding to a loudspeaker that emits the sound via an amplifier, and a battery as a power source. By using an implemented interface, hearing aids for bone conduction forward the sound directly to the bones of the skull via the mastoid.