NOISE IS OFTEN AN UNWANTED STIMULUS to the body, and clear links have been established between prolonged exposure to noise and shorter life expectancy (Maynard & Moorhouse, 2009). Good acoustic design is often seen as simply controlling disturbance and maintaining privacy. In healthcare buildings, good acoustic design is of greater importance because it can affect the health and recovery of the patients using the building. High noise levels not only cause obvious effects like annoyance and sleep disturbance but also decrease the rate at which patients’ wounds heal and increase the likelihood of rehospitalization. Links have also been found between noise exposure of staff and increased levels of stress, fatigue, and emotional exhaustion (Anjali & Ulrich, 2007). This is in addition to the usual communication difficulties associated with any noisy environment.
With regards to privacy there are few environments where maintaining confidentiality is of such importance. Architects and designers in the US should be aware that it is a federal government requirement to ensure that healthcare organizations provide privacy for patient health information. This extends to any spoken information and so it becomes directly linked to the acoustic performance of the building.
8.2.1 Performance specifications
Healthcare buildings are often unique in their acoustic requirements due to the very nature of the building’s use. With high levels of mechanical and electrical services, controlling noise from the building becomes a particular issue. Much of the machinery and many tasks undertaken within healthcare buildings require controlled environments and this often extends to the control of noise and even vibration. Finally, providing privacy, confidentiality, and comfort are paramount but often conflict with the nature and use of the building.
The three key design goals for healthcare buildings are as follows:
 controlling noise affecting patient and staff areas from either external noise sources or noise sources associated with the building,
controlling noise affecting patient and staff areas from either external noise sources or noise sources associated with the building,
 providing partitions within the building that will ensure that confidentiality is maintained, as well as enhancing the control of possible noise disturbance,
providing partitions within the building that will ensure that confidentiality is maintained, as well as enhancing the control of possible noise disturbance,
 providing suitable levels of control with regards to room acoustics without compromising clinical standards and performance.
providing suitable levels of control with regards to room acoustics without compromising clinical standards and performance.
Specific guideline levels for airborne sound insulation, ambient noise control, acceptable mechanical noise levels, and impact insulation requirements are detailed in Appendix B.
8.2.2 Sound insulation
With specific regards to sound insulation of partitions:
 Locating rooms adjacent to one another that result in a minimum partition requirement of STC/Rw of 64 dB should be avoided.
Locating rooms adjacent to one another that result in a minimum partition requirement of STC/Rw of 64 dB should be avoided.
 For long-term health care facilities, e.g., residential care, performance specifications for walls and floors should be in line with local building codes/standards associated with separating partitions between dwellings.
For long-term health care facilities, e.g., residential care, performance specifications for walls and floors should be in line with local building codes/standards associated with separating partitions between dwellings.
 It should be remembered that loud speech is not uncommon in treatment and consultation rooms, so good levels of acoustic insulation are of paramount importance if privacy is to be protected.
It should be remembered that loud speech is not uncommon in treatment and consultation rooms, so good levels of acoustic insulation are of paramount importance if privacy is to be protected.
8.2.3 Controlling reverberation
Reverberation times are not commonly set as performance standards in healthcare buildings, due to often conflicting clinical requirements. It is considered good practice to ensure that:
 An area equivalent to 80 percent of the floor should be covered with a material which provides a minimum NRC/absorption coefficient of 0.95.
An area equivalent to 80 percent of the floor should be covered with a material which provides a minimum NRC/absorption coefficient of 0.95.
 Where this cannot be achieved the acoustic performance of any separating partition either side of the room should be increased by 3 dB.
Where this cannot be achieved the acoustic performance of any separating partition either side of the room should be increased by 3 dB.
For non-clinical areas, such as administrative or conference accommodation, guidelines for offices or educational buildings can be followed. Large open atrium or circulation areas are likely to require specialized acoustic design.
8.2.4 External noise limits
External areas used by staff, patients, or the public, such as accessible courtyards or landscaped areas, should be designed so that noise from services associated with the hospital does not exceed the existing daytime background level (LA90) or is not higher than LA90 50 dB, whichever is highest.
When considering the design of mental healthcare facilities, it is not unusual for the location to be chosen based on the tranquil nature of the existing environment. For outdoor treatment or relaxation areas, upper average noise limits of LAeq 50–55 dB during the daytime should be targeted.
Mechanical noise from the healthcare building should be controlled to a level which does not exceed LAeq 65 dB at the healthcare building façade and controlled to the pre-existing ambient noise level at the nearest noise sensitive location (e.g. dwelling), whichever is lowest.
Heliports should be located such that noise levels do not exceed LAeq 80 dB at the nearest noise sensitive location (e.g., dwelling). This assumes limited use of the heliport, i.e., fewer than three flights per day and no more than two flights during the nighttime period (10:00 PM–7:00 AM).
Emergency generator noise should be controlled to a level of LAeq 70 dB when measured at the façade of the healthcare building.
8.2.5 Internal doors and openings
Table 8.1 outlines suggested performance requirements for openings in internal walls, along with specification information and suitable locations. Doors to store cupboards and similar ancillary space would not require an acoustically rated door.
Table 8.1 Suggested performance requirements for openings in walls
Opening type | Suggested specification | Expected performance rating STC/Rw dB | Suitable location |
Standard door | Timber/metal door (light 44 mm @ 27 kg/m2) | 30 | • Staff offices, meeting rooms, etc. to corridors • Ancillary rooms to corridors |
Enhanced door | Timber/metal door (heavy 54 mm @ 29 kg/m2) | 35 | • Any medical treatment or consultation rooms to corridors or adjoining space |
Unrated vision panel | Single layer of glass in sliding frame | n/a | • Where visual and verbal communication is required, e.g., reception desk to waiting room |
Standard vision panel | 10 mm float glass/12 mm cavity/6.4 mm laminate glass | 40 | • Glazing set into a corridor wall or door frame between a medical treatment space and circulation space where some verbal communication is required |
Enhanced vision panel | 6mm float glass/100 mm cavity/4 mm float glass | 45 | • Where visual communication is required between a medical treatment space and another room, e.g., operating theater to observation gallery |
Optimum vision panel | 10 mm float glass/200 mm cavity/6 mm laminated glass (absorptive lining to window reveal between panes of glass) | 49 | • Between highly noise-sensitive areas and adjoining spaces, e.g., infant ICU and visitor gallery or treatment and observation rooms |
 Rubberized seals are likely to be more clinically suitable than felt or brush seals.
Rubberized seals are likely to be more clinically suitable than felt or brush seals.
 Infection control designers should be consulted on the use of door seals.
Infection control designers should be consulted on the use of door seals.
 It may not be possible to accommodate seals in doors which swing both ways or double doors, as compressible seals may require a rebate.
It may not be possible to accommodate seals in doors which swing both ways or double doors, as compressible seals may require a rebate.
 Drop-down seals are likely to cause issues for rooms where trolley access is required.
Drop-down seals are likely to cause issues for rooms where trolley access is required.
8.2.6 Maximum permissible noise levels
Noise intrusion from external sources and noise from other parts of the building should be controlled to below LAmax(f) 45 dB within rooms where patients may be sleeping, and LAmax(f) 50 dB for operating rooms.
8.3.1 Controlling external noise
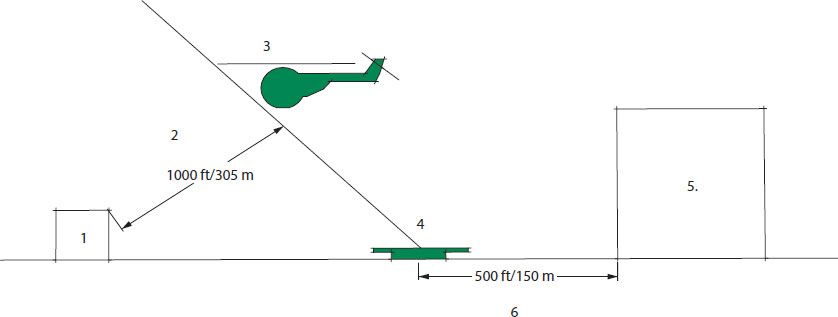
Heliports: Figure 8.1 details the suggested positioning for a hospital heliport, assuming it is located on the ground. For heliports located on the roof of a hospital, it would be necessary to ensure that no treatment/consultant rooms, patient sleeping areas, operating rooms or noise-sensitive laboratory equipment is located on the floor directly below the heliport and any room within 20 ft (6 m) of the helipad. Where possible, heliports should be located on top of ancillary space such as mechanical rooms and as remote from the core healthcare activities as possible. Specialist guidance on façade and roof specifications should be sought for roof-mounted heliports.
1) Nearest dwelling or noise-sensitive location
2) Minimum slant distance between noise-sensitive location and helicopter
3) Helicopter takeoff flight path
4) Helipad
5) Hospital
6) Minimum standoff distance between heliport and hospital building
(see Figure 8.1)
8.1 Heliport location
Road and rail noise: It is advisable to ensure that any rooms specifically for the treatment or care of patients, along with any noise-sensitive rooms (e.g., operating rooms), are a minimum of 65 ft (20 m) from any road or railway line. Control of noise break-in to such areas will be reliant upon design; therefore it is likely that mechanical ventilation will be required as allowing for open windows for ventilation would not be an option. The general principles on building location and layouts outlined in Chapter 4 and Chapter 7 should be consulted.
Courtyards are often a popular design feature of healthcare developments due to the size of the building. These can provide quiet areas around which noise-sensitive rooms can be clustered and allow for natural ventilation to rooms. In such areas, the following is advised:
 Windows should be top-hinged, bottom-hinged, or sash and case opening to limit noise ingress and reduce noise egress from a room.
Windows should be top-hinged, bottom-hinged, or sash and case opening to limit noise ingress and reduce noise egress from a room.
 If the courtyards are to be accessible to staff, patients or visitors, placing noise-sensitive rooms or rooms where patient privacy is important at ground-floor level, should be avoided.
If the courtyards are to be accessible to staff, patients or visitors, placing noise-sensitive rooms or rooms where patient privacy is important at ground-floor level, should be avoided.
 Placing seating directly against the façade of any courtyard should be avoided, to maintain privacy to rooms which overlook the space.
Placing seating directly against the façade of any courtyard should be avoided, to maintain privacy to rooms which overlook the space.
 The use of dense soft planting and soft landscaping should be encouraged in order to limit noise buildup within the courtyard.
The use of dense soft planting and soft landscaping should be encouraged in order to limit noise buildup within the courtyard.
 Mechanical or electrical rooms should not be located within or overlooking any courtyard which has noise-sensitive rooms located around it.
Mechanical or electrical rooms should not be located within or overlooking any courtyard which has noise-sensitive rooms located around it.
Rain noise should be controlled so that it does not increase the target ambient noise level within any space by 20 dB. Guidelines on roof specifications are given in Chapter 4.
External mechanical rooms such as rooftop equipment associated with the building should be located away from patient treatment areas. It is often advisable to spread the location of rooftop equipment across the roof rather than gathered in a single location, to avoid noise buildup. Locating rooftop equipment areas towards façades where existing noise levels are higher (e.g., those overlooking a road) can help to mask the overall noise buildup. An allowance in rooftop equipment design should be made for the inclusion of an acoustic barrier, such as a louvered acoustic screen or solid barrier with an absorptive internal face. Guidelines on such screens are given in Chapter 4.
8.3.2 Room adjacencies to avoid
The room adjacencies detailed in Table 8.2 should be avoided.
Table 8.2 Room adjacencies to avoid
Room | Room |
Main kitchen/delivery rooms/nurseries | |
Nurseries | Archive rooms/lecture theaters/chapel/multisensory rooms/speech therapy/operating rooms |
Delivery rooms | Archive rooms/lecture theaters/chapel/multisensory rooms/speech therapy |
Multisensory rooms/speech therapy rooms | Main kitchen/nurseries/delivery rooms |
Chapel | Main kitchen/nurseries/delivery rooms |
Main kitchen | Archive rooms/lecture theaters/operating rooms/multi-sensory rooms/speech therapy rooms/chapel |
Note: Placing patient treatment or consultation rooms below either heavily trafficked areas (e.g., corridors) or physiotherapy gyms should be avoided.
8.3.3 Room layout
The following guidelines on planning and room massing are suggested:
 Group service activities, such as laundries, main kitchens, main stores and mechanical rooms, together so that they can be located away from noise-sensitive space (treatment/consultation rooms, etc.). This will help reducing noise impact from the activities within these rooms, as well as noise associated with mail deliveries and waste disposal.
Group service activities, such as laundries, main kitchens, main stores and mechanical rooms, together so that they can be located away from noise-sensitive space (treatment/consultation rooms, etc.). This will help reducing noise impact from the activities within these rooms, as well as noise associated with mail deliveries and waste disposal.
 Avoid placing noise-sensitive rooms so that they have a direct view of any primary service areas (e.g., waste stores, loading bays).
Avoid placing noise-sensitive rooms so that they have a direct view of any primary service areas (e.g., waste stores, loading bays).
 Locate imaging equipment (e.g., MRI) at ground-floor level and away from noise-sensitive locations. This will help reduce any impact from noise and vibration from such equipment, while also reducing any potential interference from unwanted vibration from external sources.
Locate imaging equipment (e.g., MRI) at ground-floor level and away from noise-sensitive locations. This will help reduce any impact from noise and vibration from such equipment, while also reducing any potential interference from unwanted vibration from external sources.
 Operating rooms should be positioned in a quiet part of the building away from any heavy traffic areas. Sudden high noise events should be controlled as far as it is practical.
Operating rooms should be positioned in a quiet part of the building away from any heavy traffic areas. Sudden high noise events should be controlled as far as it is practical.
 Allowing for a separate mechanical building to accommodate HVAC units can significantly reduce mechanical noise issues.
Allowing for a separate mechanical building to accommodate HVAC units can significantly reduce mechanical noise issues.
 Including smaller, multiple nurses’ stations rather than large nurses’ stations can help reduce noise buildup around hospital wards and treatment areas.
Including smaller, multiple nurses’ stations rather than large nurses’ stations can help reduce noise buildup around hospital wards and treatment areas.
 Include buffer zones between waiting areas and treatment/consultation rooms. Bathroom facilities, as well as doors, between waiting areas and corridors to treatment rooms are possible solutions.
Include buffer zones between waiting areas and treatment/consultation rooms. Bathroom facilities, as well as doors, between waiting areas and corridors to treatment rooms are possible solutions.
 Avoid placing treatment or consultation rooms directly off main circulation routes or in close proximity to café/dining spaces.
Avoid placing treatment or consultation rooms directly off main circulation routes or in close proximity to café/dining spaces.
 Where possible, the provision of single bed wards should be encouraged over multi-bed wards, as they have been found to reduce recovery times for patients.
Where possible, the provision of single bed wards should be encouraged over multi-bed wards, as they have been found to reduce recovery times for patients.
 For large or medium-sized wards as well as admittance areas (e.g., emergency rooms) include small meeting rooms to allow for confidential discussion between patients, visitors, and medical staff.
For large or medium-sized wards as well as admittance areas (e.g., emergency rooms) include small meeting rooms to allow for confidential discussion between patients, visitors, and medical staff.
 Service and passenger lifts/elevators should be located well away from any noise-sensitive room. They will also have to be separated from any vibration-sensitive laboratory or medical equipment.
Service and passenger lifts/elevators should be located well away from any noise-sensitive room. They will also have to be separated from any vibration-sensitive laboratory or medical equipment.
8.3.4 Room design
 Avoid the use of interconnecting doors between treatment/consultation rooms. Entrance doors to consulting or treatment rooms should be located as far apart as possible. Glazed panels to the side of a door but within the doorframe are likely to reduce the overall performance of a partition and should only be included for operational reasons.
Avoid the use of interconnecting doors between treatment/consultation rooms. Entrance doors to consulting or treatment rooms should be located as far apart as possible. Glazed panels to the side of a door but within the doorframe are likely to reduce the overall performance of a partition and should only be included for operational reasons.
 Screen off areas within wards or nurses’ stations which are used for preparing medication or completing patient charts. Three-sided booths can be useful, as they can provide some screening as well as clearly defining an area where tasks requiring high levels of concentration are undertaken.
Screen off areas within wards or nurses’ stations which are used for preparing medication or completing patient charts. Three-sided booths can be useful, as they can provide some screening as well as clearly defining an area where tasks requiring high levels of concentration are undertaken.
 Allow for the provision of secluded or withdrawn areas off corridors or wards. This allows for visitors to find informal spaces to hold semi-private discussions or congregate prior to, or after, visiting periods without causing significant disturbance to patients.
Allow for the provision of secluded or withdrawn areas off corridors or wards. This allows for visitors to find informal spaces to hold semi-private discussions or congregate prior to, or after, visiting periods without causing significant disturbance to patients.
 The use of positive air pressure rooms in intensive care units can be useful in controlling the spread of infection as well as separating potential noisy observation areas from patients.
The use of positive air pressure rooms in intensive care units can be useful in controlling the spread of infection as well as separating potential noisy observation areas from patients.
8.3.5 Sound masking
The principles of sound masking are discussed in Chapter 3. Sound masking can be a useful way of covering noise which patients and staff may find disturbing, and it is often worth considering for very quiet sites. Sound masking has been used successfully in the following types of spaces:
 mental health wards or social interaction spaces in residential care facilities
mental health wards or social interaction spaces in residential care facilities
 any space where there are multiple treatment cubicles (e.g. curtains)
any space where there are multiple treatment cubicles (e.g. curtains)
 large to medium-sized office space
large to medium-sized office space
 waiting areas
waiting areas
 large to medium-sized wards
large to medium-sized wards
 treatment/examination rooms
treatment/examination rooms
 spaces close to delivering or maternity rooms.
spaces close to delivering or maternity rooms.
Masking levels of LAeq 48 dB are generally accepted as reasonable during daytime periods. For wards or areas where sleeping may occur this level will have to be adjusted for nighttime periods. This will depend on the underlying noise level on site but reductions of 10 dB between daytime and nighttime are expected to be reasonable. Active masking systems are available which adjust to the ambient noise level within the room as it changes.
Note: the inclusion of an effective noise masking system may allow for the acoustic performance of separating partitions to be reduced by 5 dB. This would not apply to delivery or maternity rooms.
8.3.6 Ducted air services
Healthcare buildings are usually heavily serviced buildings requiring substantial design allowances for air conditioning equipment.
 As outlined in Figure 7.4, where possible main service ducts should be run along corridors and enter rooms via the corridor wall. Running services directly through walls which separate noise-sensitive rooms should be avoided.
As outlined in Figure 7.4, where possible main service ducts should be run along corridors and enter rooms via the corridor wall. Running services directly through walls which separate noise-sensitive rooms should be avoided.
 It is anticipated that any Mechanical and Electrical (M&E) contractor will be expected to provide mechanical equipment which does not give rise to noise levels which exceed the guidance on noise levels given in Appendix B.
It is anticipated that any Mechanical and Electrical (M&E) contractor will be expected to provide mechanical equipment which does not give rise to noise levels which exceed the guidance on noise levels given in Appendix B.
 The use of an acoustically attenuating ceiling tile should be considered in any design (e.g., ceilings with a minimum rating of CAC 35 or Dn,c,,w 35 dB).
The use of an acoustically attenuating ceiling tile should be considered in any design (e.g., ceilings with a minimum rating of CAC 35 or Dn,c,,w 35 dB).
 Cross-talk attenuators should be allowed for in ducts which service two or more rooms. These normally take the form of attenuators placed within the duct or flexible lined duct sections.
Cross-talk attenuators should be allowed for in ducts which service two or more rooms. These normally take the form of attenuators placed within the duct or flexible lined duct sections.
 Introducing bends in a duct system can help reduce noise breakout at the grill. Note: bends in duct systems can lead to noise breakout levels increasing at other locations, and so wrapping the duct in a mass layer with an absorptive lining should also be considered. Additional bends may also require higher levels of air pressure through an AC system.
Introducing bends in a duct system can help reduce noise breakout at the grill. Note: bends in duct systems can lead to noise breakout levels increasing at other locations, and so wrapping the duct in a mass layer with an absorptive lining should also be considered. Additional bends may also require higher levels of air pressure through an AC system.
 Standard duct attenuation methods are often not feasible in healthcare buildings due to clinical requirements. The use of bagged/sealed absorptive materials or non-fibrous materials may need to be considered or allowances may need to be made for significant space provision for fresh air plenums to ducting systems (i.e., large boxes located prior to duct terminations which help reduce air noise through a ventilation system).
Standard duct attenuation methods are often not feasible in healthcare buildings due to clinical requirements. The use of bagged/sealed absorptive materials or non-fibrous materials may need to be considered or allowances may need to be made for significant space provision for fresh air plenums to ducting systems (i.e., large boxes located prior to duct terminations which help reduce air noise through a ventilation system).
 Air transfer grills at duct system terminations should be selected on their acoustic performance.
Air transfer grills at duct system terminations should be selected on their acoustic performance.
8.3.7 Electrical, gas and water services
 The use of flashing light alarms rather than audible alarms is preferable for emergency alarm systems in intensive care or infant care units. It is, however, expected that this will have to be cleared with any health and safety requirements.
The use of flashing light alarms rather than audible alarms is preferable for emergency alarm systems in intensive care or infant care units. It is, however, expected that this will have to be cleared with any health and safety requirements.
 Silent ringing telephones are also preferable in intensive care or infant care units.
Silent ringing telephones are also preferable in intensive care or infant care units.
 Gas and air outlets along with electrical sockets and switches should ideally be mounted on service panels rather than being cored out of any separating partition. Placing such services back to back on either side of a partition should also be avoided.
Gas and air outlets along with electrical sockets and switches should ideally be mounted on service panels rather than being cored out of any separating partition. Placing such services back to back on either side of a partition should also be avoided.
 Heating pipes and water pipes should be fitted with resilient mounts in areas where they are fixed to partitions within rooms used for sleeping.
Heating pipes and water pipes should be fitted with resilient mounts in areas where they are fixed to partitions within rooms used for sleeping.
8.3.8 Vibration and impact noise
The control of vibration is a complex subject and where necessary specialist advice should be sought. The nature of the equipment used in health care buildings often means that particular care should be taken when dealing with vibration sources. The following outlines general guidelines on this subject in relation to the control of structure-borne sound.
 Full concrete constructions have been found to provide better inherent levels of vibration control than steel and concrete composite constructions.
Full concrete constructions have been found to provide better inherent levels of vibration control than steel and concrete composite constructions.
 Composite steel and concrete constructions can achieve good levels of vibration control but usually require the overall mass of the floor to be almost double that required for purely structural reasons.
Composite steel and concrete constructions can achieve good levels of vibration control but usually require the overall mass of the floor to be almost double that required for purely structural reasons.
 It is unlikely that suitable levels of vibration can be achieved from lightweight timber floor structures without the inclusion of significant additional mass and isolation (e.g., concrete screeds and proprietorial isolation systems).
It is unlikely that suitable levels of vibration can be achieved from lightweight timber floor structures without the inclusion of significant additional mass and isolation (e.g., concrete screeds and proprietorial isolation systems).
 Table 8.3 outlines suitable vibration control levels for a range of room types. These levels do not guarantee complete control of vibration particularly for specialist medical and laboratory equipment. The guidelines given in the table allow for average performance levels but should be seen as performance levels for any individual event rather than an average for hypersensitive areas such as operating rooms and specialist laboratories.
Table 8.3 outlines suitable vibration control levels for a range of room types. These levels do not guarantee complete control of vibration particularly for specialist medical and laboratory equipment. The guidelines given in the table allow for average performance levels but should be seen as performance levels for any individual event rather than an average for hypersensitive areas such as operating rooms and specialist laboratories.
 Irregularities in floor surface (e.g., threshold bars and expansion joints) should be minimized or located in low traffic areas to reduce noise from trolleys and wheeled beds.
Irregularities in floor surface (e.g., threshold bars and expansion joints) should be minimized or located in low traffic areas to reduce noise from trolleys and wheeled beds.
 Rubberized flooring, resilient underlay, or backing for vinyl flooring can help to reduce footfall noise as well as limit vibration from trolleys and wheeled beds. (Note: Resilient underlay or backings can be prone to puncture so care should be taken when specifying.)
Rubberized flooring, resilient underlay, or backing for vinyl flooring can help to reduce footfall noise as well as limit vibration from trolleys and wheeled beds. (Note: Resilient underlay or backings can be prone to puncture so care should be taken when specifying.)
Table 8.3 Suggested vibration control levels (adapted from Cavanaugh et al. 2006 and Concrete Centre, 2004)
Room | Acceleration (RMS 1 sec) | Vibration peak velocity (micro-in/s) |
(Wg Frequency Weighting) | ||
Wards | 0.2ms–1.75 | 2000 |
Treatment areas | 0.4ms–0.75 | 4000 |
Offices/consultation | 0.8ms–1.75 | 8000 |
8.3.9 Clinical requirements and room finishes
The following recommendations are given:
 In clinical areas, the use of cleanable absorptive ceilings is desirable. Ceiling tiles that can be pressure- or steam-washed, and/or wall panels with an impermeable layer such as a vinyl finish, are preferable.
In clinical areas, the use of cleanable absorptive ceilings is desirable. Ceiling tiles that can be pressure- or steam-washed, and/or wall panels with an impermeable layer such as a vinyl finish, are preferable.
 The use of ceiling systems which include anti-microbial films on their exposed surfaces is advisable for clinical areas.
The use of ceiling systems which include anti-microbial films on their exposed surfaces is advisable for clinical areas.
 Ceiling- or wall-mount absorptive finishes which include any horizontal surface which could allow for dust or dirt to gather should be avoided. Fix wall-mounted panels hard against the joint between the wall and the ceiling to avoid the creation of a horizontal surface.
Ceiling- or wall-mount absorptive finishes which include any horizontal surface which could allow for dust or dirt to gather should be avoided. Fix wall-mounted panels hard against the joint between the wall and the ceiling to avoid the creation of a horizontal surface.
 Avoid suspended ceiling grids in mental healthcare units in favor of perforated plasterboard ceilings or surface-mounted absorptive tiles/panels.
Avoid suspended ceiling grids in mental healthcare units in favor of perforated plasterboard ceilings or surface-mounted absorptive tiles/panels.
 The use of standard acoustically absorptive materials in non-clinical areas is normally permissible. For spaces such as atria, it is likely that the same approach as that outlined for school atria can be adopted.
The use of standard acoustically absorptive materials in non-clinical areas is normally permissible. For spaces such as atria, it is likely that the same approach as that outlined for school atria can be adopted.
 Consider including additional absorption in noise-sensitive areas within larger spaces, e.g., nurses’ stations or areas where medicine is prepared or medical charts are filled in.
Consider including additional absorption in noise-sensitive areas within larger spaces, e.g., nurses’ stations or areas where medicine is prepared or medical charts are filled in.
8.3.10 Separating partitions
Specification details for good practice when constructing separating walls and floors are given in the drawings in Appendix C.
Note: Where it is not possible to meet the minimum acoustic absorption requirements (set out in Table 8.4), then the level of insulation for the partitions in these areas should be increased by 3 dB.
8.3.11 Room finishes
Table 8.4 outlines suggested wall, floor, and ceiling finishes to ensure the control of reverberation and good speech intelligibility within a variety of healthcare type rooms, άw are given for ceiling and wall panel finishes. Suitable material types may be limited due to clinical requirements. Appendix C includes possible finishes.
Table 8.4 Recommended floor, wall, and ceiling finishes by material or absorption coefficient άw (healthcare)
Room description | Floor άw | Ceiling finish άw | Wall άw |
Clinical spaces | |||
Ward (single/multi-person) | Unrated cleanable finish | 0.65–0.8 over full ceiling (allowance for lighting) | Unrated cleanable finish |
Mental healthcare/long-term care | Unrated cleanable finish | 0.65 over full ceiling assumed perforated plasterboard or bonded tiles | Unrated cleanable finish |
Medical treatment (operating theaters/MRI/ultrasound) | Unrated cleanable finish | 0.65–0.95 over full ceiling (allowance for lighting); lower performance specification permissible if clinical requirements dictate | Unrated cleanable finish |
Intensive care/recover room (ICU/infant care) | Unrated cleanable finish | 0.85–0.9 over full ceiling (allowance for lighting) | Unrated cleanable finish |
Consultation rooms | Unrated cleanable finish | 0.9 over full ceiling (allowance for lighting) | Unrated cleanable finish |
Non-clinical areas | |||
Changing rooms | Vinyl flooring unrated | 0.8 over full ceiling area (allowance for lighting) | Plaster or tile |
Corridors/stairwells | Vinyl flooring unrated | 0.9 over full ceiling area (allowance for lighting) | Plaster or painted brick/block |
Kitchens | Vinyl/tile unrated | 0.8 over full ceiling area | Plaster or tile |
Lecture room large >50 students | 0.3 Carpet | 0.8 over rear 75 percent of ceiling | 0.8 over 25 percent of wall distributed over the back wall and the rear of the side walls |
Lecture room small | < 50 students | 0.3 Carpet | 0.8 over 50 percent of ceiling 0.8 over 25 percent of walls located to rear of room |
Record rooms | 0.3 Carpet | 0.9 over full ceiling (allowance for lighting) | Plaster finish |
0.3 Carpet | 0.8 over 50 percent of ceiling | 0.8 over 25 percent of wall area | |
Laboratories | Vinyl unrated | 0.8 over full ceiling (allowance for lighting) | Plaster/painted block finish |
Toilets/showers | Vinyl flooring unrated | 0.8 over full ceiling (allowance for lighting) | Plaster or tile |
Anjali, J., and Ulrich, R. (2007) Sound control for improved outcomes in healthcare settings. Concord, CA: Centre for Health Care Design.
Cavanaugh, W. J., et al. (2006) Draft interim sound and vibration design guidelines for hospitals and healthcare facilities. Acoustical Society of America/Institute of Noise Control Engineering/National Council of Acoustical Consultants.
Ceilings and Interior Systems Construction Association (CISCA) (2010) Acoustics in healthcare Environments. Oak Brook, IL: CISCA.
Concrete Centre (2004) Hospital floor vibration study. Comparison of possible hospital floor structures with respect to NHS vibration criteria. London: Ove Arup & Partners.
Department of Health (2013) Specialist services – health technical memorandum, 08-01: Acoustics. London: Department of Health.
James, A., and Zoontjens, L. (2012) Helicopter noise impacts on hospital development design. Proceedings of Acoustics 2012, November 21–23, Fremantle, Australia, Australian Acoustical Society.
Maynard, R., and Moorhouse, A. (2009) Environmental noise and health in the UK. London: Health Protection Agency/Public Health England.